In a classic comic strip, most recently gracing the Beano, tiny characters called “numskulls” live in the head of a chap called Edd, controlling what he gets up to – often with hilarious results. It has run for decades, presumably because the idea that there could be critters within us capable of exerting a profound mental and physical influence seems pretty absurd.
But it appears science is having the last laugh: in recent years the idea has spawned myriad research papers – except that instead of minuscule people at work inside one’s head, it is microbes in the gut that appear to be pulling the strings.
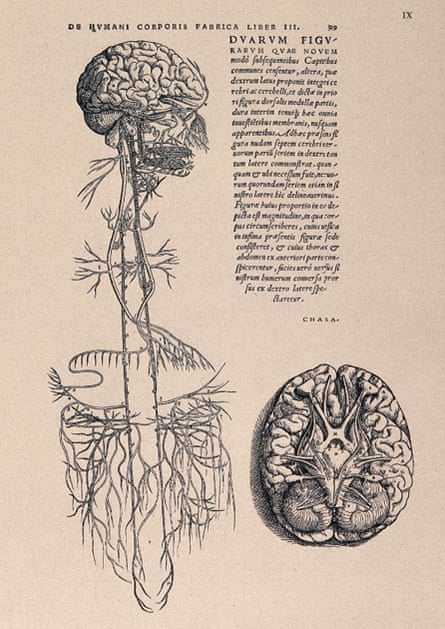
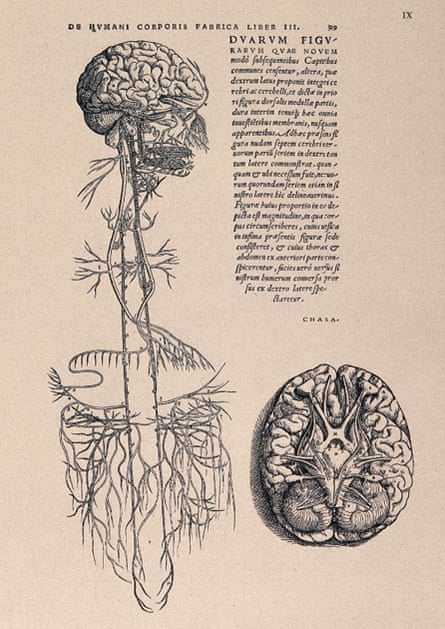
How microbes in the gut influence the brain – and vice versa – is still being unpicked. Studies have revealed possible routes of communication that include the immune system, branches of the vagus nerve that run from the gut to the brain, and interaction with the nerves and synapses that control the function of the gastrointestinal tract. If the links could be understood, and harnessed, experts say the impact could be profound.
Scientists hope that by shifting the composition of microbes in the gut, either by administering particular microbes or helping beneficial microbes to thrive, they may be able to help treat disorders such as anxiety and depression – an approach known as psychobiotics.
“A large percentage of people who take medication or psychotherapy to treat mild or moderate [cases] don’t respond,” says Prof John Cryan of University College Cork, a key figure in the field, who is working on how modifying gut bacteria might be beneficial alongside other treatments.
This bold idea is bolstered by decades of research revealing what has been dubbed the “microbiota gut-brain axis”.
Many experiments have involved taking germ-free mice – animals raised in a sterile environment with no microbes – and introducing “good” bacteria to their insides, resulting in a reduction in stress, anxiety and depression.
But while the results are exciting, there is a complication. “Mouse and human microbiota are hugely different,” says Bhismadev Chakrabarti, professor of neuroscience and mental health at the University of Reading.
Yet evidence is growing that our own gut microbes may exert a powerful influence on our brains. Early small studies, some industry funded, found that consumption of probiotics – good bacteria such as bifidobacteria and lactobacilli – might reduce psychological distress and even affect brain activity in regions involved in controlling the processing of emotion and sensation.
One study found that taking a probiotic was associated with a reduction in negative mood. Another found that administering Bifidobacterium longum to patients with irritable bowel syndrome reduced depression, while 2022 research found that gut microbes are associated with levels of depressive symptoms.
There is even evidence that gut microbes affect neurodegenerative diseases, such as amyotrophic lateral sclerosis (ALS): one study found mice with a similar disease deteriorate faster if they do not have a gut microbiome, while introducing the bacterium Akkermansia muciniphila appeared to have a beneficial effect on their behaviour and neurological motor abilities by increasing levels of vitamin B3. Intriguingly, low levels of vitamin B3 have been found in human ALS patients, and clinical trials involving B3 supplements are being planned.
For Cryan, the concept that microbes could play a key role in psychological and neurological conditions is not a surprise. “There has never been a time where the brain has existed without microbial signals. We have evolved with these friends, and they are friends with benefits,” he says.
Questions remain about which microbes might influence which disorders, and whether it is the microbes themselves, or the chemicals they produce, that are affecting the brain.
And as Cryan notes, multiple chemicals may be at play – while their influence might shift over time. “What might be playing a bigger role in early life may play less of a role in adults,” he says.
In addition, scientists are still trying to understand what is cause and what is effect. “People with depression may change their eating habits,” says Dr Philip Burnet, a neuroscientist in the department of psychiatry at the University of Oxford. “They may not even eat much at all if they’re severely depressed. So you don’t know what that’s doing to the gut anyway.”
There are also big variations in the gut microbiomes between individuals, thanks to differences in diet, the internal environment – for example inflammation, alterations in the mucus layer, or levels of various chemicals – and genetics.
Cryan says that has a flipside: “We might be able to get tailored treatments for people to manage their own mental health,” he says.
The potential of the field is tantalising.
“We did a study where we took microbes from young animals and gave them to old animals and that was able to reverse the effects of ageing on the brain,” Cryan adds. Work in humans is already progressing. Cryan and colleagues published research last year in which they put together a diet of fermented foods, whole grains, legumes, and fruits and vegetables, such as apples, bananas, leeks and onions, that are rich in fibres that fuel the growth of good bacteria.
The team found that adults who followed this diet for four weeks had a significant reduction in perceived stress, unlike those who followed a control diet. Intriguingly, the microbes detected in the gut of the participants were similar, but the chemicals they produced changed.
Burnet is also exploring how mental health can benefit from manipulating gut bacteria. He and colleagues have found that prebiotics improved problem-solving in people with psychosis, possibly by making the brain more responsive to the antipsychotic drugs.
In another recent study, a team in the US gave adolescents with autism a drug to “mop up” gut chemicals that appear to occur at higher levels in people with the disorder. The approach was associated with reduced anxiety and irritability after eight weeks of treatment.
A key area of research is understanding the mechanisms that link gut microbes and the brain to understand why some people respond to interventions while others do not. Chakrabarti is recruiting for the largest gut and brain imaging study in humans so far, with a focus on the neurotransmitter gamma-aminobutyric acid (Gaba). Gaba is produced in the brain, and is involved in early neurodevelopment, as well as the ability for us to stop ourselves doing things – like brakes on a car. Changes in levels of Gaba have been linked to schizophrenia, autism, depression and anxiety.
The study will give participants either a placebo or a probiotic that contains bacteria that produce Gaba in the gut, then the team will measure participants’ brain activity and behaviour. The study, says Chakrabarti, aims to find out how certain gut bacteria might exert an influence on the brain.
Since our diets are in our own hands, should we try psychobiotics at home?

Cryan thinks there are positive steps that we can take, such as increasing our intake of dietary fibre – a prebiotic that promotes the growth of good bacteria. These lead to the production of substances that appear to be lacking in people with depression. Fermented foods like sauerkraut, kimchi, kefir, yoghurt, as well as colourful vegetables and nuts rich in polyphenols, have been shown to be beneficial to the microbiome.
“Then there are certain things you could decrease if you are sensitive to stress, anxiety, etc,” he says. “Try to remove as much processed food as you can because a lot of it contains sweeteners, artificial emulsifiers and other things that we know are not good for our microbiome.”
It sounds like a standard healthy diet. Can we be sure the benefits are not just down to its impact on other organs, like the heart? “Good heart health is good brain health,” says Prof Jane Foster, an expert in how microbiota influence the brain from McMaster University, Canada. “But we cannot discount the potential role of microbes in improving all of that.”
Certainly the science suggests that manipulating the gut microbiome involves more than simply swallowing a dose of good bacteria. “If the person’s only eating hotdogs, it doesn’t matter how much probiotics you put in there,” she adds. “The diversity of your diet leads the diversity of your gut.”